Breast cancer impacts more than 4,000 women in Scotland per annum and remains one of the global leading causes of female cancer-related morbidity and mortality. Beyond the clinical management of patients diagnosed with breast cancer, support structures are provided via referral and signposting to additional cancer care services (e.g., Maggie's). It is being increasingly recognised that the collective experiences of the patient at diagnosis and following treatment is significant to their care and quality of life. Effective communication with the patient through developing their health history narrative can contribute to empathetic and personalized care, through which the patient is empowered and involved in their care decisions, and their lived experiences are valued. Moreover, narrative medicine can serve as a tool for training the next generation of empathetic healthcare professionals.
Why use storytelling in obtaining patient breast cancer narratives?
Storytelling is a tool that can be used in healthcare to inform patients about the innovation and design of new services and healthcare solutions. In this process, the emotions surrounding a situation, the setting, and those impacted can be used to capture different narratives of lived experiences and how these contribute to individual experiences. All stories were structured using the three act structure (Story arc:1) starting with a beginning (introduction to the patient and where their breast cancer story began), progressing onto a middle stage (what were the experiences defining the story) and ending with a conclusion (wrap-up and the present day), with periods of reflection factored into each stage.
The storytelling workshop series
To celebrate Scotland’s year of Stories 2022, the authors collaborated with an oral historian, Yvonne McFadden and a professional storyteller, Allison Galbraith. Together, we co-developed a three-part storytelling workshop in which every participant would contribute to the event in order to create a patient-carer-clinician-scientist cohort. Narratives were gradually developed over the course of the first two workshops using roundtable discussions, icebreakers, presentations from scientists, object memories or storytelling prompt cards. Each workshop was developed with a theme in mind, developing the following three sessions:
- Workshop 1: An introduction to storytelling
- Workshop 2: Bringing your story to life
- Workshop 3: Open-mic storytelling
More than 20 patient participants and six scientists currently involved in breast cancer research attended all three workshop sessions. All participants, including scientists as well as clinicians developed their own narratives and perspectives on breast cancer.
All the stories were captured and recorded in multiple media formats including audio recordings, digital images and artwork. Each audio story has been carefully transcribed. This information will be used to produce legacy content and support resources for patients diagnosed with breast cancer.
We found that storytelling within an informal workshop setting provided a friendly forum for patients to connect with each other in a safe space. This enabled them to explore their emotions and feelings about being diagnosed with cancer. It also led to many of the patients sharing their experiences with each other, from diagnosis through to treatment, and life after cancer. For many of the participants, it was the first time they had openly shared details of their cancer experience.
We found that using a structured workshop approach spanning three sessions, patient participants and their carers were able to develop their stories for delivery via open-mic format to fellow patient and scientist participants. The gradual structure used for the workshop activities started with the use of object memories and histories to capture the relevance of an item in an individual’s cancer journey. Discussing the value and relevance of the object within the personal journey provided a means within small groups to reflect on similarities and differences between their own lived experiences of breast cancer.

Fig. 1- Object gallery representing the range of objects used to develop patient and scientist narratives of breast cancer
In the second session while patients were made aware of ongoing research efforts to develop new diagnostics and treatments, their own narratives were further structured via prompts to capture various stages of their breast cancer journey.
Fig. 2- Storytelling prompt cards used in workshop 2, to develop the start, middle and end stages of the patient narratives on their breast cancer lived experiences.
Lessons Learned
Qualitative feedback was captured from all participants including patients and scientists. Their feedback are included below (fig 3):
“When the multidisciplinary team (MDT) process was described at the workshop, it made me feel safe knowing that my case is being discussed in detail as a person. It was great to hear about the process.”
“Attending the workshop series made me see the patient as opposed to breast cancer cell lines I research, which don’t have a voice. When I continue with my research, I will be thinking more about the patient that will benefit from my work.”
“I attended the event as the husband of a breast cancer survivor and would encourage other husbands/partners to attend future events. The day was educational, interesting and inspiring, and I am pleased that I chose to attend. I loved learning other women’s stories and have a huge admiration for the bravery, stoicism, and humour that they demonstrated when discussing their own personal experiences.”
Our initial analysis of the narratives collected showed that patient care for those diagnosed with breast cancer continues long after their involvement with the clinic and treatment. This is notably a significant improvement in patient prognosis and outcomes. Themes that emerged from the patients who participated include stories focussed on (1) lack of autonomy in treatment decisions, (2) deficiency in awareness of different types of breast cancer, (3) competing caring responsibilities and (4) survivorship guilt. Earlier and more widespread narrative oncology interventions with patients at point of diagnosis and referral to resources can better support patient care and continue with the growth of this innovative patient-centred approach to cancer treatment. Following positive feedback from all participants, we plan to continue this project to include more patients with breast cancer, including more underrepresented voices in breast cancer (male patients, Black, Asian and minority ethnic patients) in our future efforts.
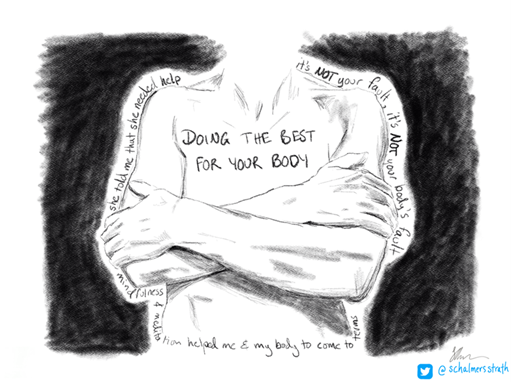
Fig. 3. Artistic visualization of patient perspectives on their body image following a breast cancer diagnosis
Definitions:
Storytelling: Storytelling is the interactive art of using words and actions to reveal the elements and images of a story while encouraging the listener’s imagination.
Narrative medicine (Charon et al): The medicine practiced with the narrative competence to recognize, absorb, interpret and be moved by the stories of illness.
Comments
If you are a British Pharmacological Society member, please
sign in to post comments.