‘A growing rep and curing strep – the rise of community pharmacy’ is the 2021 winning article from our annual writing competition for early career pharmacologists. It was written by Abbie Thomas from Swansea University Medical School. Our judges enjoyed Abbie’s submission’s flowing, articulate exploration of an important topic.
For each writing competition, we look for exceptionally written and well-communicated science on any pharmacology-related topic. Each of our entries was scored independently by a panel of judges*.
How a healthcare project in Wales is using pharmacists to treat sore throats and tackle antibiotic resistance
This is unlikely to be the first time you have read or heard that General Practitioners (GPs) across the UK are struggling to meet the increasing demands of a growing population, and I for one never cease to be amazed at how they manage such a staggering workload. Utilising the vast teams of allied healthcare professionals can help to ease the pressure facing General Practice, and in Wales in 2018, a pilot project aptly named ‘Sore Throat Test and Treat’, was launched with the hope of doing just that.
If you have ever had to visit your GP for a sore throat, then you certainly are not alone. It is estimated that 180,000 of us will book an appointment with our family doctor each year because we are struggling to manage the symptoms of a sore throat.
But what exactly is a sore throat?
Perhaps you are a doctor, a scientist, or just really into your medical terms, and know what is meant by the term ‘pharyngitis’. Even if you are unfamiliar with the term, you have still probably experienced it and know it by its common description – a sore throat.
Acute pharyngitis and tonsilitis are both conditions that can cause swelling, pain and redness in different areas of the mouth. With pharyngitis, the infection will be deep down in your throat, most likely further than your eyes can see. Tonsilitis, as the name suggests, is in your tonsils (if you have them), which are the two large bump-like structures at either side of the back of your mouth, as labelled in the image below. Although after a year of COVID-19 tests, you may be able to find your tonsils in your sleep!

Figure 1. “Tonsil” by Freepik / CC by 3.0
Infections in the throat can be caused by bacteria, or a virus, and this makes a difference to the treatment needed. Viruses and bacteria are tiny living organisms that can cause us to become ill by entering our bodies, without us knowing, and multiplying. It is worth noting that not all bacteria are bad, in fact most are harmless. When I say they are tiny, I really mean it. It is said that the rhinovirus (the virus that causes the common cold) is so small that 500 million of them would be able to fit onto the head of a pin.
Unfortunately, if your sore throat is caused by a virus then there is little your GP can do, other than advise you to take painkillers if required, drink lots of water, and get plenty of rest. If the infection is caused by bacteria, then it is likely to be a type of bacteria called Streptococus pyogenes. This little organism is notorious for getting under our skin and into our throats to make us ill, and just like the viral infection, your GP will probably advise you to rest up and drink up. However, scientists of the past and present have worked tirelessly to discover something that has the potential to help you get rid of those pesky bacteria - enter antibiotics.
But are antibiotics ‘the pill for every ill’?
The discovery of the first antibiotic, penicillin, by Sir Alexander Flemming in 1928 is a prime example of a triumph in medical science that has ultimately lengthened lives. Antibiotics work by killing bacteria, not viruses, preventing them from multiplying and the infection worsening. Sadly, as a society we were blissfully unaware of how precious antibiotics were and began to use them as ‘the pill for every ill’. We know now that the more we use antibiotics, the less effective they become. This is because bacteria are clever, and just like us, they are able to make changes that increase their ability to survive against new and existing threats – this warrants a whole blog post in itself, so please follow this link if you are interested in finding out how they do this.
Bacteria have learned how to protect themselves from antibiotics, and the World Health Organisation have now warned that antibiotic resistance is one of the biggest threats to global health today. There is no back-up plan to antibiotics. If they are no longer able to kill bacteria before infections become serious or even fatal, then we have no way of stopping them. This impacts anyone and everyone – that bacterial sore throat we discussed above? Well, that could leave you in hospital. Let’s not flower things up here, antibiotic resistance means that previously minor, easily treatable infections could be life-threatening.
How do antibiotics kill bacteria?
Different antibiotics have different ways of killing bacteria and making sure our immune systems are stronger than the bacteria. One of these mechanisms is shown below.
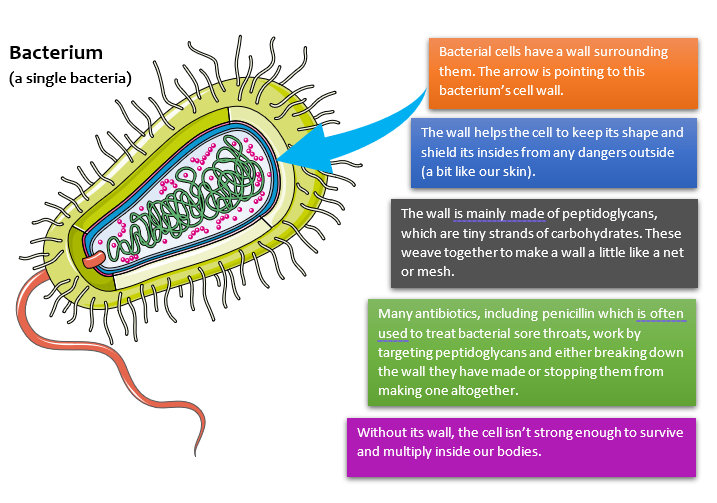
Figure 2. “Bacterium” by Servier Medical Art / CC BY 3.0
Helping the NHS to help you
Here is where the ‘Sore Throat Test and Treat’ scheme comes in. In 2016, 122,000 prescriptions of antibiotics were issued to medicate a sore throat. This is likely to have been more than necessary, but minimising antibiotic resistance is all of our responsibilities. Recognising that the pressures facing GPs may be a factor in overprescribing, the Welsh government and NHS enlisted the help of community pharmacies.
The ‘Sore Throat Test and Treat’ scheme means that someone with a sore throat can bypass the need for a GP appointment and head straight to their community pharmacy. Their throat will be examined by a pharmacist, a highly skilled and qualified healthcare professional, and a swab taken from their throat to test for the presence of the bacteria discussed above, Streptococus pyogenes. The pharmacist will then carry out tests on the swab and will be able to tell within minutes whether the sore throat is caused by the bacteria or a virus. This means that they can accurately decide the best form of treatment and prescribe antibiotics only when the bacteria are confirmed as the cause.
This started as a pilot project in just two Welsh health boards, with the aims of decreasing unnecessary antibiotic use, decreasing GP consultations, and improving patient care. It proved to be a roaring success and reduced antibiotic prescriptions for sore throats by 65%!
Now available across all health boards in Wales**, the scheme is a shining example of how care in the community paves the way to more easily accessible and effective healthcare and the invaluable potential of community pharmacy to help achieve this. It would be great to see the success of this project lead to community pharmacy being used far more in government plans for the future of NHS care and the fight against antibiotic resistance. Remember to consider using your local pharmacy from now on – they may well offer many services that you didn’t know about.
*This year’s judging panel was made up of: Craig Daly (Pharmacology Matters editor), Hannah Roughley (Pharmacology Matters editor), James Boncan (Pharmacology Matters editor), Josh Dignam (Pharmacology Matters editor), Lauren Taylor (Pharmacology Matters editor), Sorrel Bunting (then Engagement Manager at the Society), Taichi Ochi (Pharmacology Matters editor), and Sarah Bailey (Vice President Engagement at the Society).
**Please check with pharmacies in your area as availability may vary between providers and the scheme is beginning to appear in other UK nations.
Comments
If you are a British Pharmacological Society member, please
sign in to post comments.