Published: 12 May 2021
Category:

Please note: this article discusses the use of offensive and discriminatory language.
Mental health can touch people in different ways, including through personal experience or through caring for someone with a mental health problem. Mental health problems can have debilitating impacts on the lives of those affected, but they are often invisible, and so the full impacts are not always obvious. Whilst it is encouraging to see mental health stigma improve for some conditions, both social and self-stigma remains high with schizophrenia. This can influence recovery and lead to relapses. We need to do more to break the taboo around schizophrenia. For my undergraduate project, I wanted to look beyond the textbook coverage of schizophrenia, explore current public perceptions, and engage with people who have personal experiences of schizophrenia.
Symptoms and treatment
Globally, schizophrenia affects 20 million people and is thought to impact 1 in every 100 people at some point in their lives. Schizophrenia is characterised by symptoms of psychosis, where people experience delusions and auditory hallucinations (known as positive symptoms), along with a lack of motivation and a loss of interest (known as negative symptoms). People can also experience cognitive difficulties, with impairments in working memory and attention. Schizophrenia is a complex condition with no sole cause, however both genetic (nature) and environmental (nurture) factors such as trauma, brain development issues and birth defects might contribute to its development. In the clinical management of schizophrenia, therapies are currently limited to symptomatic treatment to improve the quality of life for patients and it is well recognised that social, biological, and psychological factors are important when considering the available treatment options. Doctors usually prescribe anti-psychotic drugs to manage positive symptoms. Cognitive behavioural therapy (CBT) can also be helpful.
Since developing chlorpromazine in the 1950s, researchers have continued to make major efforts to alter the progression of schizophrenia and learning more about the causes of schizophrenia helps us to create new therapies. Although numerous anti-psychotic drugs are currently in clinical use, their side effects are not always well tolerated and treatment-resistant schizophrenia (TRS) may occur in up to 34% of patients. Furthermore, current medications do not substantially improve the negative symptoms and cognitive difficulties. Given these challenges for treatment, it is disheartening to think that stigmatisation could make the path to recovery even more complicated. This is such an important aspect of the inequality that surrounds mental health problems compared to physical health problems. We also need to address the lack of resources for developing medications to reduce schizophrenia’s debilitating side effects.
Living with schizophrenia: the stigma
In 2012, the Schizophrenia Commission (formed through Rethink Mental Illness) published a report called The Abandoned Illness. The report explained the barriers to UK healthcare access, highlighted important areas of concern and made recommendations for improvements. Stigma was one of the major issues impacting healthcare experiences for people with schizophrenia. In 2014, Support in Mind Scotland - in collaboration with the University of Edinburgh - published the results of the ‘1 in 100’ Scottish schizophrenia survey. This report provided valuable insights into the lives of people with schizophrenia from their own perspectives and through the perspectives of carers and family members of people with the condition. The report explored topics such as stigma, care, treatment, wellbeing, and quality of life. Stigma associated with schizophrenia can prevent people from openly sharing their experiences. Negative portrayals of mental health problems and language used by the media can create additional misunderstanding and public fear of conditions like schizophrenia. The fear of judgement and subsequent inability to confide in others may prevent those with schizophrenia from accessing essential healthcare for early intervention and recovery. In the last 20 years, campaigns geared to reduce mental health stigma, such as Open the Doors and Time to Change, have made positive impacts on public attitudes to mental health problems.
What is the first thing you think of when you hear the word schizophrenia?
To understand the current public perception of schizophrenia, I created a survey on social media, which asked ‘what is the first thing you think of when you hear the word schizophrenia?’. I received anonymous responses from 127 people, and I used these responses to create the word cloud in Figure 1. I found that many respondents connected schizophrenia with mental health. I also found that many respondents had negative connotations of schizophrenia, as some associated it with words like ’unstable’, ‘psycho’, ’crazy’, ‘scary’ and ‘mad’. These results emphasised the lack of understanding and the prevalence of misconceptions about the disease. These factors contribute to the social stigma attached to schizophrenia. Some respondents submitted terms relating to positive symptoms of schizophrenia, such as ‘voices’ and ‘hallucinations’, however fewer people submitted terms relating to the negative symptoms. Some respondents entered words like ‘misunderstood’, ‘stigma’ and ‘badly portrayed’, showing that they were aware of the wider issues people with schizophrenia face beyond the clinical symptoms.
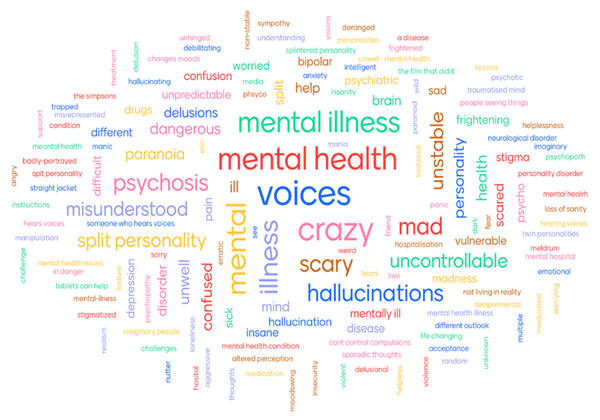
Figure 1. Word association of schizophrenia – a public perspective. I used Mentimeter to survey the public and shared the link via social media. I posed the question ‘What is the first thing you think about when you hear the word ‘schizophrenia’?’ Each respondent could submit up to 3 words and all entries were anonymous. The larger the font size, the more respondents entered that word. The survey was open for 48 hours and I received responses from 127 people within this timeframe.
Living with schizophrenia: the rich picture
I conducted follow-up interviews with people with lived and carer experience of schizophrenia. These testimonies painted a richer picture of the condition. They showed how misconceptions and stigmas can impact people living with schizophrenia. We can see that the experience of diagnosis is not necessarily a negative one and that young people with schizophrenia are just the same as others of their age - they are hopeful and ambitious for their future.
Here are some quotes from my interviews:
I was 21 when I received my diagnosis and I felt a little relieved if I’m honest. It made me feel better that there was a name for what I had been going through. I haven’t had any symptoms since December 2017. I had a lot of negative experiences with the medications. I am currently at college and I plan to continue my studies at university.
- Student with lived experience of schizophrenia
I was a teenager when I realised that my mum had schizophrenia. Although she experienced recurrent episodes with frequent hospitalisation and relapse, she was a talented knitter with so much creativity and impressive needle skill. She initially chose to keep her diagnosis to herself because she did not want to be defined by her illness. As she got older, she became less concerned about stigma and was more open with people about her diagnosis.
- Dr Margaret Cunningham, University of Strathclyde
People often think that episodes for schizophrenia are manic, and wild displays of aggressive behaviour. This is where schizophrenia is misunderstood. It can also be silent episodes but those are the type you rarely hear about.
- Carer for a parent with schizophrenia
Stakeholder network: driving change with multidisciplinary input
I established a network of people across disciplines with interests in schizophrenia. This network is currently made up of design researchers, a schizophrenia researcher, a historian, a community pharmacy, a mental health charity and advocates with carer and lived experiences of schizophrenia. Through the project, the team identified an opportunity to change the narrative around schizophrenia. We wanted to capture and share these more positive and humanising experiences of living with the condition through digital storytelling. The Physiological Society recently awarded an outreach grant to the network to support engagement and the creation of digital resources for storytelling - to amplify the voices and talents of people living with schizophrenia.
Who is currently involved in the network?
 |
Elio Caccavale
Elio Caccavale is a Reader in Transdisciplinary Design Innovation at the Glasgow School of Art. Elio is investigating design and science partnerships, and new visual and three-dimensional design vocabularies for thinking about ethical and social issues in the sciences.
|
 |
Frances Simpson
Frances Simpson is the Chief Executive of Support in Mind Scotland, which is a national charity working to improve the wellbeing and quality of lives of people affected by serious mental health problems. This includes those who are family members, carers, and supporters.
|
 |
Judith Pratt
Judith Pratt is a Neuroscience Research Professor at the University of Strathclyde. Judith’s expertise is in preclinical translational research focusing on the causes of mental health problems. Her research seeks to understand genetic and environmental factors for schizophrenia and autism to inform new treatments.
|
 |
Margaret Cunningham
Margaret Cunningham is a Senior Lecturer in pharmacology at the University of Strathclyde with experience of growing up with a parent with schizophrenia.
|
 |
Michael Pierre Johnson
Michael Pierre Johnson is a postdoctoral design researcher at the Glasgow School of Art. Michael uses design practices, such as visual mapping and modelling methods, to support and evaluate creative collaboration between different experts, stakeholders, and the public, in the face of shared societal challenges.
|
 |
Natalie Weir
Natalie Weir is a Research Associate at the University of Strathclyde with a key interest in patient safety and implementation science. Natalie works part time as a community pharmacist.
|
 |
Yvonne McFadden
Yvonne McFadden is an oral historian based at the Scottish Oral History Centre at the University of Strathclyde. Currently, she is a Research Associate on the Lost Villages of East Ayrshire, which looks at housing, community, gender, and health in the lost miner’s row villages.
|
Other members of this growing network include Andrew Stevenson, Sally Cunningham and Stephanie Allan. If you are interested in getting involved or want to find out more about the project, then please email: margaret.cunningham@strath.ac.uk
Comments
If you are a British Pharmacological Society member, please
sign in to post comments.