Published: 13 Aug 2020
Category:
In May 2020, the Prescribing Safety Assessment partnership won the Royal College of Physicians' Excellence in Patient Care Award for medical education and training. This blog is also published on the RCP website.
A critical aspect of clinical governance in healthcare is to ensure safe prescribing. Medicines are a major tool to treat disease and relieve suffering, but also have the potential to cause significant harm. Around 7–10% of prescriptions written by trainee doctors in UK hospitals contain errors, with similar rates reported internationally. In England, there are an estimated 50 million prescribing errors annually. Many factors contribute to prescribing errors, including the prescribing environment, the complexity of modern medicines, and sub-optimal prescribing practices. Studies suggest that new graduates often feel underprepared and anxious about prescribing, a concern echoed by their supervisors.
The
British Pharmacological Society and
Medical Schools Council established the multi-stakeholder
Safe Prescribing Working Group in 2007 to better prepare graduates for the challenge of prescribing. This led to the creation of the
Prescribing Safety Assessment (PSA). Work began in 2010 when there were no precedents for a prescribing assessment on this scale. All UK medical schools were involved, pooling academic resources to deliver a high-quality assessment applied equitably to all students, matching GMC learning outcomes, unifying prescribing standards and ultimately improving prescribing education. The entire PSA process, from item authoring to results release, is managed online. Although this was a novel and challenging approach in 2010, the widespread deployment of electronic prescribing systems in recent years has proved that decision to be prescient.
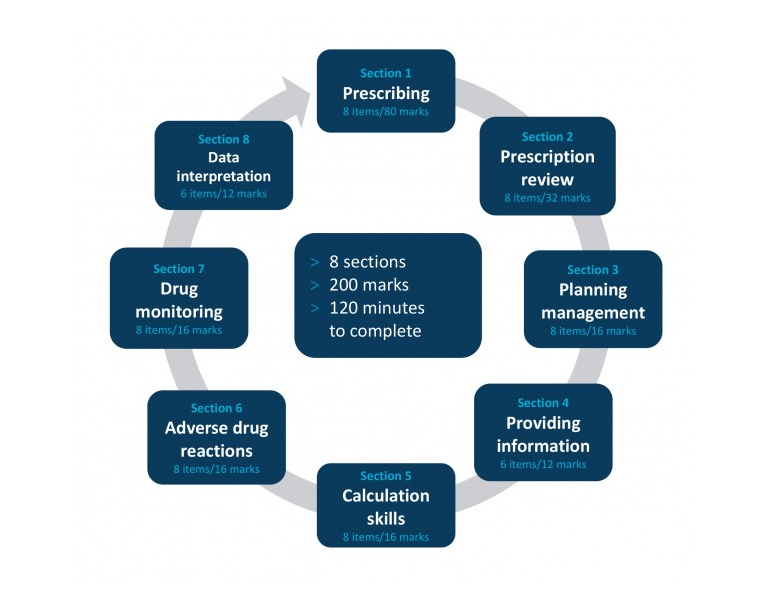
The PSA blueprint comprises eight sections, reflecting different aspects of the prescribing process (see figure). The question items are based on 60 patient scenarios in seven clinical domains, with 200 marks available during a 2-hour assessment.
PSA question items are written by doctors and pharmacists and undergo a stringent quality assurance process, overseen by the PSA Assessment Board. Items that survive each stage of review are entered into the PSA item bank, which includes around 3,500 items. The pass mark is determined by a Standard-Setting Group (using the modified Angoff method) with knowledge of the minimum standard expected of FY1 doctors.
PSA summative assessments are delivered live from a cloud-based server to timed events under invigilated conditions. Following a post-assessment review, results are released directly to candidates. Around 100,000 prescriptions are automatically marked in each annual cycle.
The PSA was implemented across all UK medical schools in 2014 and in foundation schools in 2016. It is challenging to prove that patient outcomes have improved as a direct result of the PSA because of multiple confounding factors. However, there is evidence of improvement in candidate performance:
- pass rates have steadily increased
- the variation in performance between medical school cohorts has reduced
- performance of candidates on similar items has progressively improved
There has undoubtedly been additional focus on prescribing education in an effort to ensure that students are better prepared to pass. Psychometric analysis showed that PSA papers delivered in 2019 had a Cronbach’s alpha of 0.80 or above.
Candidate feedback indicates that the PSA is an acceptable test of prescribing competence, that the scenarios are relevant to the work of a foundation doctor, and that preparing for and taking the PSA is a valuable experience.
In 2019, an external review of the quality and impact of the PSA concluded that it meets international acceptable standards of good assessment practice; stakeholders believe it is having a positive educational impact, and increases the attention paid by students and faculty to accurate prescribing. The executive summary concluded that ‘while no single test could be a determinant of patient safety, the PSA is almost certainly a significant contributor to patient safety.’
The PSA is an excellent example of innovation in UK medical education. It is the first large-scale national prescribing assessment and is probably one of the largest online medical assessments in the world. Critical elements have been:
- the willingness of UK medical schools to collaborate
- UK strengths in clinical pharmacology, pharmacy and medical education
- availability of national prescribing competency frameworks
- national statements on evidence-based prescribing (BNF, NICE)
The innovative approach and reputation for excellence of the PSA attracts international attention. It has now been adapted for delivery to undergraduate and postgraduate doctors and pharmacists around the world. The PSA, or variants of it, have been run in 1,555 events in 166 institutions to over 60,000 candidates.
Winning the RCP EPCA 2020 for medical education provides welcome recognition of the innovation and impact of the PSA.
Comments
If you are a British Pharmacological Society member, please
sign in to post comments.