The Medicines and Healthcare products Regulatory Agency (MHRA) has issued new advice, concluding a possible link between the Oxford-AstraZeneca COVID-19 vaccine and extremely rare, unlikely-to-occur blood clots.
Whilst the MHRA advises that careful consideration be given to people who are at higher risk of specific types of blood clots, the regulator said that overall, the benefits of the Oxford-AstraZeneca vaccine outweigh the risks. Noting the need to make decisions based on the relative benefits versus the risks in different age groups, the Joint Committee on Vaccination and Immunisation (JCVI) also stated that those in the 18-29 age group will be offered an alternative vaccine.
The refinement of advice was described as a ‘course correction’ by Deputy Chief Medical Officer, Professor Jonathan Van Tam and as a reasonable and expected response to gathering new data. The ability to respond to new data demonstrates the value of UK monitoring systems for ongoing pharmacovigilance (for example through the MHRA Yellow Card Scheme) as an important process for monitoring new therapeutics as they are used at scale, in larger populations. While clinical trials can detect common adverse effects, extremely rare ones can only be detected when larger populations are studied.
The European Medicines Agency also concluded their review on the vaccine this afternoon, stating that the overall balance of benefit versus risks remains positive.
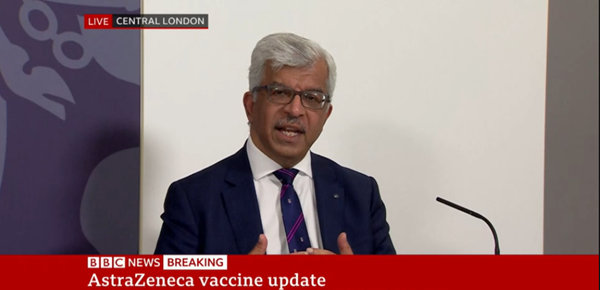
Speaking at a joint MHRA and JCVI press conference, Professor Sir Munir Pirmohamed, President of the Society and Chair of the Commission on Human Medicines, outlined the Commission on Human Medicines advice:
“We have worked with the Commission on Human Medicines and expert working group separately to thoroughly review all the cases coming in with the Oxford-AstraZeneca vaccine. We’ve taken into account a wide range of data sources, we’ve looked at information about usage of the vaccine in various age groups, updated incidents rates and risks comparisons by age and gender."
"Each report has been carefully scrutinised by the MHRA and by the members of the working group, and further information has been obtained where necessary. We’ve also had independent adjudication of these cases by an expert haematologist, and we worked with another group of haematologists to develop a case definition of these events to make sure the cases were identified throughout the UK and reported via the Yellow card scheme."
"Based on the currently available data the Commission on Human Medicines advises the following:
- Pregnant women should continue to discuss with their healthcare professional whether the benefits of having the vaccine outweigh the risks for them
- People with a history of blood disorders that increase the risk of clotting should only have the Oxford-AstraZeneca COVID-19 vaccine when the benefits outweigh any potential risks
- Anyone who experiences cerebral or other major blood clots occurring together with low levels of platelets after the first Oxford-AstraZeneca COVID-19 vaccine should not have the second dose
We will be continually monitoring further reports as they come in, [and] continually monitoring other aspects to identify risks factors so we can refine the advice that we give. At present, the data on people who have had two doses of the Oxford-AstraZeneca COVID-19 vaccine are limited because these events are rare. A comparatively small number of second doses have been given. Therefore, it is not possible to draw a conclusion about how frequently blood clots with a low platelet count happen following a second dose of the vaccine, but this will be monitored closely by the MHRA and the CHM as part of the ongoing review."
To put it into context, these events are extremely rare, as Dr June Raine has already mentioned. I also want to put it into context in relation to COVID-19 itself. It is important to remember that COVID-19 causes clotting, and it causes lowered platelets.
"I have a few figures from a recent paper published. pulmonary embolism (clots on the lungs) occur in 7.8% of people who have COVID-19, deep vein thrombosis (clots in the legs) occur in 11.2% who have had COVID-19. Of those people infected with SARScov2, getting COVID-19, and ending up in the ITU, 23% will have some form of clot. COVID-19 also causes strokes in about 1.6%, and up to 30% of people who get COVID-19 will get thrombocytopenia, which is lowering of the platelet count. That puts into context the risks of clots and lower platelets is much higher with COVID-19 than these extremely rare events occurring with the vaccine."
"To finish, the CHM has advised that the link between the vaccine and blood clots in the cerebral and other veins, occurring together with lower platelets, is getting firmer, but absolute proof between the vaccine and adverse events will need extensive scientific work."
Based on the currently available evidence, the benefit risk remains favourable for the vast majority of people, but it is more finally balanced for the younger people and we are advising that this evolving evidence should be taken into account when considering the use of the vaccine.
In response to further questions about use of the vaccine in younger age groups, Sir Munir said:
“There is a slightly higher risk in the younger age group compared to the older age group. We do need to look at the relative benefits versus the risks in different age groups. The reasons why it’s a higher risk in the younger age group is not clear – we need to undertake much more scientific work to understand why the link between the vaccine in the younger age group is occurring. That will help us in the future to be able to refine the advice we give in terms of product information, but further work needs to be done."
“With regard to children, the trial has been paused by the data safety monitoring board for an abundance of caution. We know that children are at much lower risk of these clots and as we are able to accumulate more data over the next few weeks, the MHRA and the expert working groups will be liaising with the trialists at Oxford to determine whether the trial can start again, based on the data that are available.”
In response to further questions about understanding the link between the vaccine and these blood clots, Sir Munir said:
“The early evidence suggests that this constellation of symptoms is caused by an immune response against platelets which allows the platelets to then lead to clotting in different parts of the body. But what we don’t have clearly is the link between the vaccine and how the immune response becomes activated against the platelets, and that’s where the scientific work needs to go on – to identify what that link is, so we can develop ways and strategies to overcome this adverse event for the future.”
“There is an immune response occurring to [an unknown event], it may be the vaccine or it may be previous COVID-19 infection, for example. The way that immune response then targets platelets, and why it targets platelets in a very small number of individuals is not clear. I think it is very important to understand the mechanisms, it can provide us with ways of being able to prevent this in the future. For example, if you are able to identify the mechanisms we may be able to refine the advice that’s given so we can identify risk factors and try to prevent it in individuals that have that risk factors. It may allow us to think about modified vaccines which do not cause this particular adverse effect in the future. There are several vaccines with adenoviral vectors, but we don’t know if it’s related to the vector or something else – that’s part of the scientific work that needs to be done”.
“Of the 79 cases, 51 were in women and 28 were in men. The numbers are quite small, and this may reflect who is getting the vaccine because many of the healthcare workers are women. But if you look at the incidence rate, to the number of vaccines administered there is no difference between men and women. But at the moment we don’t have evidence to say either men or women are likely to get this.”
Update: 7 May 2021
The Joint Committee on Vaccination and Immunisation (JCVI) has
issued advice to the UK government on the use of the coronavirus (COVID-19) Oxford/AstraZeneca vaccine for people aged under 40. The JCVI has advised a preference for adults aged 30 to 39 without underlying health conditions to receive an alternative to the Oxford/AstraZeneca vaccine – where available and only if this does not cause substantial delays in being vaccinated. Professor Wei Shen Lim, COVID-19 Chair for JCVI, said:
"Safety remains our number one priority. We have continued to assess the benefit-risk balance of COVID-19 vaccines in light of UK infection rates and the latest information from the MHRA on the extremely rare event of blood clots and low platelet counts following vaccination. As COVID-19 rates continue to come under control, we are advising that adults aged 18 to 39 years with no underlying health conditions are offered an alternative to the Oxford/AstraZeneca vaccine, if available and if it does not cause delays in having the vaccine. The advice is specific to circumstances in the UK at this time and maximises use of the wide portfolio of vaccines available. The COVID-19 vaccines have already saved thousands of lives and the benefit for the majority of the population is clear – if you are offered the vaccine, you should take it."
The JCVI is advising that everybody who has already had a first dose of the Oxford/AstraZeneca vaccine should receive a second dose of the same jab, irrespective of age, except for the very small number of people who experienced blood clots with low platelet counts from their first vaccination.
To find out more about how pharmacology and clinical pharmacology have contributed during the COVID-19 pandemic, please read
our recent news story and
visit our COVID-19 news hub.