
Download this resource as a printable two-page poster.
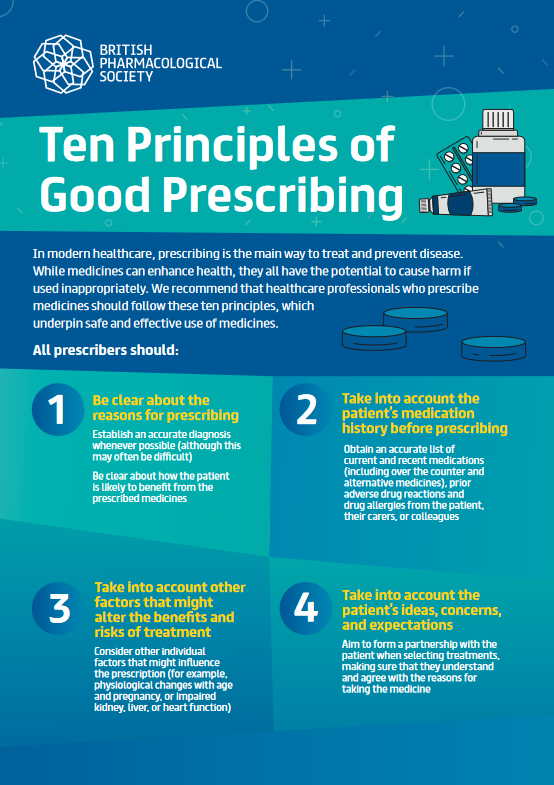
Prescribing is the main approach to the treatment and prevention of disease in modern healthcare. While medicines have the capacity to enhance health, all have the potential to cause harm if used inappropriately. We recommend that health care professionals who prescribe medicines should do so based on the following ten principles, which underpin safe and effective use of medicines.
All prescribers should:
1. Be clear about the reasons for prescribing
- Establish an accurate diagnosis whenever possible (although this may often be difficult)
- Be clear in what way the patient is likely to gain from the prescribed medicines
2. Take into account the patient’s medication history before prescribing
- Obtain an accurate list of current and recent medications (including over the counter and alternative medicines); prior adverse drug reactions; and drug allergies from the patient, their carers, or colleagues
3. Take into account other factors that might alter the benefits and risks of treatment
- Consider other individual factors that might influence the prescription (for example, physiological changes with age and pregnancy, or impaired kidney, liver or heart function)
4. Take into account the patient’s ideas, concerns, and expectations
Seek to form a partnership with the patient when selecting treatments, making sure that they understand and agree with the reasons for taking the medicine
5. Select effective, safe, and cost effective medicines individualised for the patient
- The likely beneficial effect of the medicine should outweigh the extent of any potential harms, and whenever possible this judgement should be based on published evidence
- Prescribe medicines that are unlicensed, ‘off label’, or outside standard practice only if satisfied that an alternative medicine would not meet the patient's needs (this decision will be based on evidence and/or experience of their safety and efficacy)
- Choose the best formulation, dose, frequency, route of administration, and duration of treatment
6. Adhere to national guidelines and local formularies where appropriate
- Be aware of guidance produced by respected bodies (increasingly available via decision support systems), but always consider the individual needs of the patient
- Select medicines with regard to costs and needs of other patients (health care resources are finite)
- Be able to identify, access, and use reliable and validated sources of information (for example, British National Formulary), and evaluate potentially less reliable information critically
7. Write unambiguous legal prescriptions using the correct documentation
- Be aware of common factors that cause medication errors and know how to avoid them
8. Monitor the beneficial and adverse effects of medicines
- Identify how the beneficial and adverse effects of treatment can be assessed
- Understand how to alter the prescription as a result of this information
- Know how to report adverse drug reactions (in the UK via the Yellow Card scheme)
9.Communicate and document prescribing decisions and the reasons for them
- Communicate clearly with patients, their carers, and colleagues
- Give patients important information about how to take the medicine, what benefits might arise,
- adverse effects (especially those that will require urgent review), and any monitoring that is required
- Use the health record and other means to document prescribing decisions accurately
10.Prescribe within the limitations of your knowledge, skills and experience
- Always seek to keep the knowledge and skills that are relevant to your practice up to date
- Be prepared to seek the advice and support of suitably qualified professional colleagues
- Make sure that, where appropriate, prescriptions are checked (for example, calculations of intravenous doses)