
Elizabeth Adeyeye, clinical pharmacology trainee at Barts Health NHS Trust, was a runner up from our 2021 annual writing competition for early career pharmacologists. For each writing competition, we look for exceptionally written and well-communicated science on any pharmacology-related topic. Each of our entries was scored independently by a panel of judges*.
Time and our bodies
Much of how we live our lives is governed by time. We wake up to an alarm, eat at mealtimes, work in the day, sleep at night, and the cycle continues. The prompts to do these things do not simply come from looking at the time on our clocks, watches, and phones. We have internal body clocks, our biological rhythms, that govern our functions and behaviours with the overall goal of keeping us alive and healthy.
The most important rhythms are the circadian rhythms. The word ‘circadian’ comes from the Latin circa meaning ‘about’ and diem meaning ‘a day’, and as the name suggests, this is a cycle that runs for approximately 24 hours. This rhythm is run by a sophisticated series of internal clocks controlled by a master clock in the brain called the suprachiasmatic nucleus. These clocks control messengers such as hormones, the levels and activities of which fluctuate throughout the day. Interestingly, the circadian rhythm mechanisms of newborn babies are under-developed. This is a large part of their erratic sleep patterns, which their parents are all too familiar with.
Whilst this internal rhythm exerts its control over us, it too is influenced by many external factors, the most important being light and dark. Our behaviours can also alter our circadian rhythms, causing our bodies to be out of sync with what nature has intended, such as in jet lag, by staying awake all night and following daylight saving clock changes.
Figure 1 shows some of the main biological processes and behaviours that are influenced by circadian rhythms.
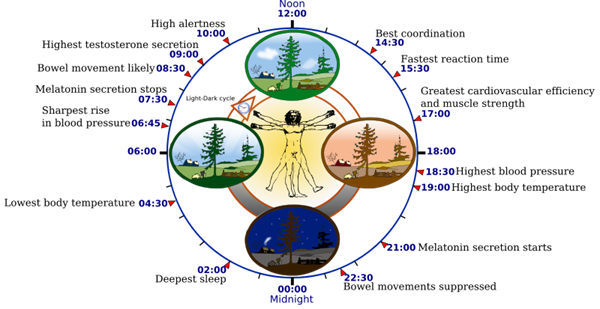
Figure 1. Biological clock human.svg by YassineMrabet. Talk fixed by Addicted04, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons.
An introduction to chronopharmacology
If our body clocks can impact our everyday functions, they could impact how our body responds to drugs. This article will focus on chronopharmacology, the study of the relationship between our internal biological rhythms and drugs. I will highlight examples of how this relationship has been used successfully in drug therapy. There are two main principles of chronopharmacology: chronopharmacokinetics, which looks at how these rhythms affect what the body does to the drug, and chronopharmacodynamics which explores the relationship these rhythms have on the effects of the drug on the body.
Chronopharmacokinetics
There are many processes that control the movement of drugs into, through and out of the body and some of these activities can vary throughout the course of a day under the influence of the circadian rhythm. For example, drugs are often broken down either to more or less active forms by a group of enzymes in the liver called the cytochrome P450 enzymes. The production of these enzymes varies throughout the day, which can affect how much active drug is available.
Chronopharmacodynamics
Many diseases show a circadian pattern in their activity. Some examples of this are demonstrated in Figure 2, which shows the time on a 24-hour clock when symptoms or events of diseases are worse or more frequent. Drugs exert their effects by acting on targets that are involved in causing the disease. This means that the effect that the drug has on these disease targets can also vary throughout the day.
.png.aspx?width=600&height=416)
Figure 2. Examples of circadian activity patterns in disease.
Chronopharmacology uses in practice and breakthroughs
We will now look at examples of how knowledge of chronopharmacology can optimise the effectiveness of a drug and reduce its harmful effects.
Asthma
The Roman physician Caelius Aurelianus was one of the first to describe night-time worsening of asthma symptoms in the fifth century, now a well recognised pattern of this condition. Theophylline, a drug that causes muscles of the airways to relax, is preferentially given at night to target this. Montelukast, which reduces inflammation in the airways, has been shown to improve asthma symptoms when given at night.
High blood pressure and heart disease
The likelihood of the blood forming clots that could potentially lead to heart attacks peaks between 6am and midday. Aspirin reduces clotting and is best given early in the morning for this reason - to prevent the formation of dangerous clots. Statins, medicines used to lower cholesterol, are more effective when given at night, as this is when cholesterol production is at its greatest. In high blood pressure treatment, large studies including the Hygia Chronotherapy Trial have shown that night-time dosing of blood pressure medications is associated with better blood pressure control and reduces the risk of serious complications such as heart disease and death.
Cancer
Perhaps the most exciting uses of chronopharmacology have been in cancer treatment, where the use of powerful and life-saving therapies is limited by their severe and debilitating side effects. One example of a major success is with oxaliplatin. This platinum-based chemotherapy agent used in bowel cancer failed in early clinical trials due to its severe toxic effects. Later, chronopharmacology studies in mice were used to test its safety. The studies revealed that giving oxaliplatin at certain times of the day – ideally at 4pm rather than early morning dosing – led to a significant reduction in its harmful effects. This information led to the drug returning to human trials, where similar results were observed. It then progressed through development and its use is now widespread. Using chronopharmacology helped save this drug from development failure and this drug has helped to save countless lives.
Time for a change?
Our understanding of the relationship of biological rhythms in disease development and drug therapy is growing. Currently however, chronopharmacology is a field that is relatively unappreciated, under-represented and under-utilised in the development of new drugs, drug regulation, and clinical practice. Given the vast financial costs and time associated with drug development, chronopharmacology could provide ways to improve the efficiency of this process, which would ultimately ensure effective medicines reach patients more rapidly. In addition, treatments already in existence may be optimised by taking chronopharmacological approaches into consideration. There is a need for more evidence to fully realise the clinical potential of chronopharmacology. William Shakespeare wrote ‘Make use of time, let not advantage slip’. With chronopharmacology, we may be able to do just that.
*This year’s judging panel was made up of: Craig Daly (Pharmacology Matters editor), Hannah Roughley (Pharmacology Matters editor), James Boncan (Pharmacology Matters editor), Josh Dignam (Pharmacology Matters editor), Lauren Taylor (Pharmacology Matters editor), Sorrel Bunting (then Engagement Manager at the Society), Taichi Ochi (Pharmacology Matters editor), and Sarah Bailey (Vice President Engagement at the Society).
Comments
If you are a British Pharmacological Society member, please
sign in to post comments.