“Herbalism is not real medicine, why are you researching that?”
This was one of the responses I received when I spoke about my final year research project on African herbalism and its use within African malarial management.
Growing up in rural Wiltshire I have been surrounded by plant enthusiasts and medical herbalism. As a scientist I have been curious in exploring the science behind ‘alternative’ medicines like herbalism. So, I was also surprised to come to the end of my biomedical based degree and have had no learning of any alternative medicine, nor any insight into worldwide medicines. I wondered why this was. My research project was the perfect opportunity to explore this area.
I stumbled across African herbalism when reading the World Health Organisation’s malarial strategy. This report featured the inclusion of integrating local and traditional methods of medicine, as currently <90% of people within Africa use herbalism as their primary source of healthcare. At present, antimalarial chemotherapies have growing issues with drug resistance and appropriate distribution across rural communities. With these two points in mind, medical herbalism could be the saviour of malarial management.
From an educational standpoint, the effective initialisation of these alternatives into mainstream care requires practitioners to be educated appropriately. As surely there is the potential of dangerous drug-drug interactions and adverse effects mixing herbal concoctions and pharmaceutical antimalarials in vulnerable people? I wanted to investigate if this education is happening already.
In light of decolonising global health systems and pharmacology, investigating African herbalism was the perfect opportunity for me to understand more about the culture surrounding African herbalism, educate myself upon the historic exploitation indigenous communities have faced and better understand the public’s perception of the topic. I understand that this is a niche area of medicine and wanted to see the influence of education and if their initial perceptions would change.
My project consisted of two questionnaires; the first distributed to university lecturers, asking if their pharmacological-based content included malaria and antimalarial African herbal remedies. The second, aimed at university personnel and the general public to investigate their perceptions of African herbalism. This also included an educational infographic about the role of herbal medicine in treating malaria, composed and written by myself, as seen below in Image 1.
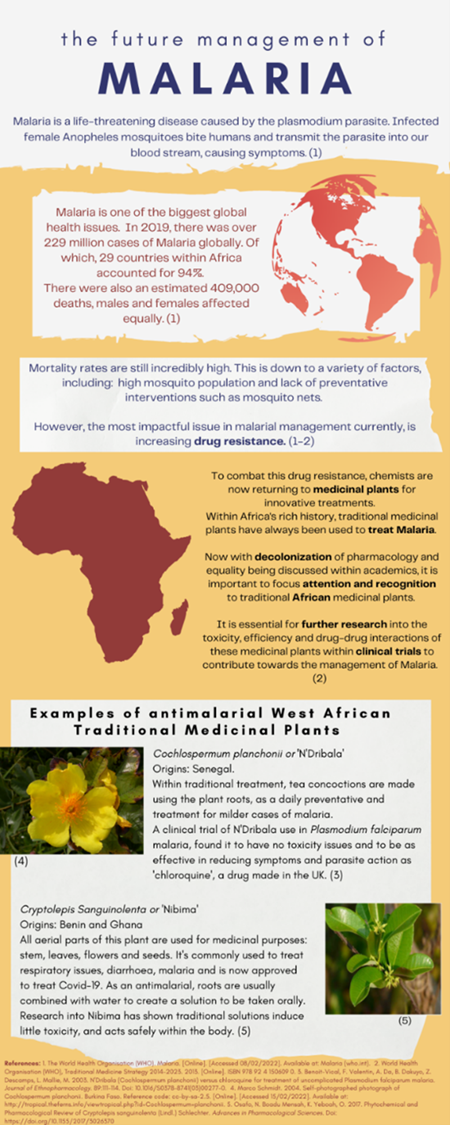
Image 1 - Educational Infographic: The infographic featured within the questionnaire that identified and measured perceptions of African medicinal plant use within malaria care. This was designed by Lucy Snow using the most recent and relevant literature. (Click image to open a large version)
Questions followed this infographic, to test if any opinions changed. The magic of social media allowed for an international response, with respondents living in USA, Nigeria, Australia etc, as seen below in Table 1.
| Category |
Frequency |
| Country |
|
| UK (and Ireland) |
71 |
| Canada |
2 |
| USA |
1 |
| Colombia |
1 |
| South Africa |
1 |
| Nigeria |
1 |
| Austria |
1 |
| Bulgaria |
1 |
| Total |
86 |
| Occupation |
|
| University student |
63 |
| Bachelor's student |
59 |
| Master's student |
6 |
| PhD |
1 |
| University Researcher or Lecturer |
9 |
| Clinician |
1 |
| Other |
14 |
| Faculty |
|
| Faculty of Medicine, Health Sciences and Veterinary Medicine |
36 |
| Faculty of Life Sciences |
6 |
| Faculty of Science |
9 |
| Faculty of Social Sciences |
15 |
| Faculty of Engineering |
1 |
| Faculty of Art |
6 |
| Other |
7 |
Table 1 - The demographic information of respondents from Questionnaire B: A table to show the demographic information e.g., geographical location, occupation, and faculty if relevant of respondents to Questionnaire B: Attitudes towards the use and education of traditional African medicinal plants, distributed via social media, n=86.
On the whole, both staff and students expressed encouragement for more research within African medicinal plants. Interestingly, most staff members had no knowledge of African antimalarial medicinal plants, but one teacher did mention Cinchona, a tree located in South America. Both staff and students showed significant change of opinion after the infographic, people became more opinionated and viewed herbalism as more of a legitimate form of medicine. An example of this is that in response to 'Effects of Traditional herbal medicines are usually the result of a placebo effect’, 26.7% of participants moved towards a greater level of disagree after the infographic, p= 0.0003.
The most interesting result gathered, was that after reading the infographic, the majority of people said they would use African medicinal plants if they were in Africa, as a form of healthcare. This data mirrors the general public of countries across Africa, and that people would and do use herbalism as medicine.
It is undisputed that now discussions into the complex decolonising issues within the world of global health. Inclusivity and equality initiatives, universities are making changes to resolve these issues. But we must ask ourselves why we as scientists are neglecting the vast area of African herbalism when thousands of people across Africa rely upon it for disease care such as malaria.
The responsibility of biomedical science and pharmacology is to investigate all medicinal forms, and prejudice must not limit this. The inclusion of alternative and traditional medicines from around the world within university curriculum would truly begin the elimination of prejudice around traditional African medicine, herbalism and decolonise pharmacology for students, academics and the general public.
Comments
If you are a British Pharmacological Society member, please
sign in to post comments.